Financial Assistance and Charity Care
Sevier County Medical Center (SCMC) is a government-owned Critical Access Hospital (CAH) existing to promote good health and provide quality healthcare with a qualified staff in a caring and compassionate manner. This hospital is committed to providing emergency care and medically necessary services to patients regardless of their ability to pay. Through our financial assistance program, we offer discounted charges for services to eligible patients that may cover all or part of their bill. The program reduces the patient bill based on income and family unit size. The reduction is based on a sliding fee scale. For uninsured patients, we will apply an automatic discount to the patient’s total charges of 40%.
A. SERVICES ELIGIBLE FOR FINANCIAL ASSISTANCE
The following healthcare services are eligible for financial assistance, depending on program eligibility:
1. Emergency medical services provided in an emergency room setting,
2. Medically necessary healthcare services,
3. Physical Therapy, Occupational Therapy, and Speech Therapy.
The following healthcare services are not eligible for financial assistance:
1. SCMC cannot offer financial assistance for the charges of any outsourced providers (not employed by SCMC) or services
such as Radiologists reading by Telerad, Blue Angels Health/Correct Care (ER Physicians), Outpatient Clinic Physicians: Cardiology, OBGYN, and lab services through AEL,
2. Services that would have been covered by government programs, commercial insurance, or other third-party payers had the patient followed the requirements of their policy and/or procedural regulations,
3. Elective procedures (not medically necessary).
The “NOTICE OF PARTICIPATING AND NON-PARTICIPATING PROVIDERS”, other than SCMC, delivering emergency or other medically necessary care in the hospital, is included within this Policy.
B. EMERGENCY SERVICES
SCMC will provide, without discrimination, care for emergency medical conditions to individuals, regardless of their eligibility under this financial assistance policy. Medically necessary care will not be delayed pending a financial assistance review
C. ELIGIBLE PATIENTS
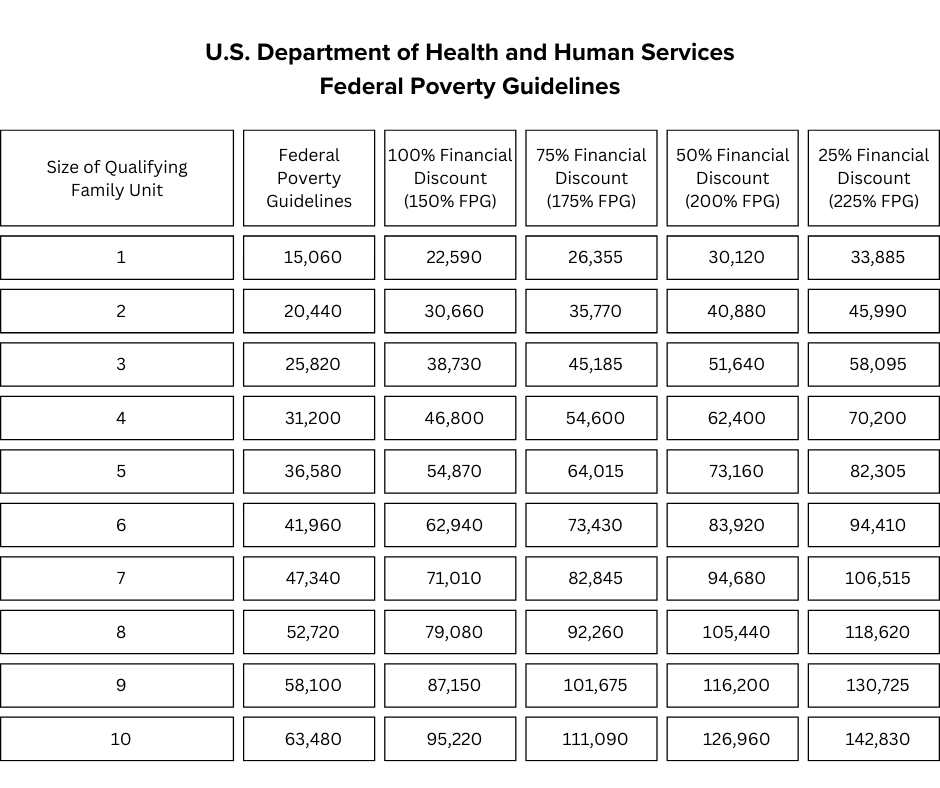
Eligibility for financial assistance will be considered for those individuals who are unable to pay for their care based upon a determination of financial need per this Policy. A person whose individual or family income is not more than 225% of the current Federal Poverty Guideline (FPG) of the United States Department of Health and Human Services may be eligible for financial assistance. An eligible patient may not be charged more than amounts generally billed (“AGB”) for emergency care or medically necessary care to individuals who have insurance. In the case of all other care provided, an eligible patient may not be charged more than the gross charges.
D. INELIGIBLE PATIENTS
Anyone who does not meet the organization’s financial assistance criteria or who refuses to provide the information necessary to determine eligibility will be determined ineligible for financial assistance.
E. DEFINITIONS:
Emergency Medical Care – Care provided by a hospital facility for emergency medical conditions.
Emergency Medical Conditions – Means emergency medical conditions as defined in section 1867 of the Social Security Act (42 U.S.C. 1395dd).
Medically Necessary Services –
1. Are consistent with the person’s symptoms, diagnosis, condition, or injury;
2. Are recognized as the prevailing standard and are consistent with generally accepted professional medical standards of the provider’s peer group;
3. Are provided in response to a life-threatening condition; to treat pain, injury, illness, or infection; to treat a condition which would result in physical or mental disability; or to achieve a level of physical or mental function consistent with prevailing standards for the diagnosis or condition;
4. Are not furnished primarily for the convenience of the person or the provider; and
5. There is no other equally effective course of treatment available or suitable for the person needing the services which is more conservative or substantially less costly.
Application Period – The period during which an application must be accepted and processed under this policy. The application begins on the date the care was provided and ends on the later of the 240th day after the date that the first post- discharge billing statement for the care is provided. Applications may be accepted outside of the application period.
Medically Indigent Person – A person whom the organization has determined is unable to pay some or all of his/her medical bills because the individual’s income is equal to or less than 150% of FPG.
Family Unit – Consists of individuals living alone; and spouses, parents, and their children under age 21 or disabled living in the same household. A family unit may include minor children living with a legal guardian.
Gross Income – Total family unit income before taxes for the most recent three (3) months. Family unit income may include earnings, unemployment compensation, workers’ compensation, Social Security, Supplemental Security Income, public assistance, veteran’s payments, survivor benefits, pension or retirement income, interest, dividends, rents, royalties, income from estates, trusts, educational assistance, alimony, child support, assistance from outside the household, and other miscellaneous sources. Noncash benefits (such as food stamps and housing subsidies) do not count. If an individual is a non- relative and living with a family, his/her income is not included in gross income.
Amounts Generally Billed (AGB) – The amounts generally billed for emergency or other medically necessary care to individuals who have insurance covering such care.
Extraordinary Collection Action (ECA) – Includes any of the following actions:
• Selling an individual’s debt to another party;
• Reporting adverse information about the individual to consumer credit reporting agencies or credit bureaus;
• Deferring, denying, or requiring a payment before providing medically necessary care because of an individual’s non- payment of one or more bills for previously provided care covered under this policy;
• Actions that require a legal or judicial process, which may include liens, foreclosure, attachment, seizure, commending a civil action, causing an individual’s arrest, causing an individual to be subject to a writ of body attachment and garnishment.
F. AMOUNT OF FINANCIAL ASSISTANCE
The hospital bill may be discounted up to 100% if the qualified patient's income does not exceed 225% of the FPG (family unit adjusted).
Patients who qualify for a reduction in their patient bill or do not financially qualify for a reduction can arrange for installment payments. After a financial assessment, the appropriate monthly payment will be assigned with a prescribed timeframe.
Sevier County Medical Center’s “NOTICE OF AVAILABILITY OF UNCOMPENSATED SERVICES” provides further details regarding the eligibility and amounts of financial assistance.
G. METHOD OF APPLYING FOR FINANCIAL ASSISTANCE AND DETERMINATION PROCEDURES
To determine if a patient is eligible for assistance, an application must be completed by the patient or guarantor. The hospital will then review the application and determine eligibility. Approval is valid for one year. Patients must apply (or reapply) for free or discounted charges with current financial information on an annual basis.
To qualify for assistance, the patient must:
• Complete an application form
• Provide documentation of gross income for the last three (3) months, including where applicable:
1. The last three pay stubs for each employed person of the qualified family unit living in the household,
2. Household members with no income should provide two letters from a relative, friend, or neighbor (not living in the household) including an explanation of how the patient’s basic financial needs are being met.
3. Copy of the last 3 months' bank statements (NOTE: Printed statements only are accepted.)
4. Most recent tax return (Form 1040) (from all adults in the qualified family unit)
5. Proof of Medicaid determination for those patients who have applied but were initially deemed ineligible for financial assistance.
Upon completion, the application and related material will be reviewed for a decision of eligibility by the Financial Counselor. Until the hospital has made reasonable efforts to determine the patient’s eligibility, we will refrain from initiating extraordinary collection activities.
An application will be considered in a “HOLD” status if a third-party coverage is discovered that will pay for the related services. The determination process will not continue until the receipt of those monies.
Upon final approval, the eligible amount will be adjusted off the patient balance and a determination letter will be mailed to the patient informing them of the results of their application. Unless the application is placed in “HOLD” status, the determination process will be completed within thirty (30) business days of receipt of the completed application.
If the application is not approved, a determination letter will be mailed to the patient informing them of the results of their application. If the patient believes the initial decision regarding his or her eligibility is incorrect, he or she may appeal the determination directly to the Revenue Cycle Manager. A decision regarding this appeal will be made within ten (10) business days.
It is preferred, but not required, that a request for financial assistance and a determination of financial need occur before rendering the non-emergent medically necessary service. The need for financial assistance shall be re-evaluated at each subsequent time of service if the last financial evaluation was completed more than one (1) year prior, or at any time additional information relevant to the eligibility of the patient for financial assistance becomes known.
H. COLLECTION ACTIONS
For patients who qualify for financial assistance and who are cooperating in good faith to resolve their discounted hospital bills, Sevier County Medical Center may offer extended payment plans. In these cases, the hospital will not send unpaid bills to outside collection agencies and will cease all collection efforts.
Sevier County Medical Center will not impose Extraordinary Collection Actions without first making reasonable efforts to determine whether that patient is eligible for charity care under this financial assistance policy except for any lien or other legal action that SCMC is entitled to assert under state law to collect payments due for medical care provided as a result of personal injuries. Reasonable efforts shall include:
1. Verifying that the patient owes the unpaid bills;
2. Providing information to the patient regarding the availability of financial assistance;
3. Providing determination of eligibility on a timely basis;
4. Determining that the hospital has pursued collections from the third-party payment sources identified by the patient;
5. Documenting that the hospital has or has attempted to offer the patient the opportunity to apply for charity care pursuant to this policy and that the patient has not complied with the hospital’s application requirements; and
6. Documentation that the patient has been offered a payment plan but has not honored the terms of that plan.
SCMC contracts with MidSouth Adjustments for its patient and/or guarantor collections. No Extraordinary Collection Action will be initiated for at least 120 days from the first post-discharge billing statement
I. MEASURES TO WIDELY PUBLICIZE FINANCIAL ASSISTANCE POLICY
Sevier County Medical Center’s Financial Assistance Policy is available to the public using various means, which may include, but is not limited to the posting of the policy:
• In the emergency room, admitting and registration departments, and patient financial service offices which are located on hospital campus locations, and at other public places as Sevier County Medical Center may elect;
• On the hospital website,
• In brochures available in patient access sites; and
• At other places within the community served by the hospital as Sevier County Medical Center may elect.
Such notices and summary information shall be provided in the primary languages spoken by the population serviced by Sevier County Medical Center. Referral of patients for financial assistance may be made by any member of the hospital staff or medical staff, including physicians, nurses, financial counselors, social workers, case managers, chaplains, and religious sponsors. A request for charity may be made by the patient or a family member, close friend, or associate of the patient, subject to application privacy laws.
NOTICE OF AVAILABILITY OF UNCOMPENSATED SERVICES
At Sevier County Medical Center, free or discounted services are available for medically necessary, non-elective inpatient and outpatient services to qualifying individuals.
ELIGIBILITY CRITERIA:
To be eligible to receive free or discounted care, your family income must not be more than 225% of the U.S. Department of Health and Human Services Federal Poverty Guidelines based unit family size.
If you think you may be eligible for free or discounted services, you may make this request at Sevier County Medical Center. A
written conditional or final determination of your eligibility will be made within thirty (30) business days of your request.
PRESUMPTIVE ELIGIBILITY
SCMC recognizes that not all patients and guarantors can complete the financial assistance application in its entirety or provide the required documentation. The hospital may, at its discretion, rely on evidence other than described throughout this policy such as, but not limited to:
1. Homeless;
2. Eligibility for other state or local assistance that is unfunded (e.g. Medicaid spend-down);
3. The patient is deceased with no known estate;
4. Medicaid eligibility
If the information above appears to lead to the conclusion that payment on the current accounts is unlikely, the manager of the revenue department will document that conclusion instead of the completed financial assistance application. Based on that conclusion, a financial assistance adjustment may be applied to the patient’s account, with the patient being notified by letter.
How to Apply:
Please feel free to reach out to our Financial Counselor at 870-584-1658 for assistance.
Our Financial Counselor will conduct a screening to determine eligibility. If necessary, the financial counselor can assist you in completing the application process. To proceed, please ensure you have the following documents ready for submission:
Valid identification (ID)
Social Security cards
Three months of recent bank statements
Three months of paycheck stubs
Your most recent tax return
If you are single and unemployed, or if both you and your spouse are unemployed, you will be required to complete a letter of no income. Additionally, please obtain three letters from non-family members confirming how you are meeting your basic needs.
Please note that the Patient Financial Counselor is available in the office from Monday to Friday, between 8:00 AM and 4:30 PM.